COVID-19 has gone big and gone global. Right now, the deadly and chaotic situation first seen in Hubei province, China in February has emerged in hotspots around the globe, including Iran, Italy, Spain, France, and New York City and its surrounds. Significant clusters are emerging in most countries around the globe and most US states. We will pass a million cases in the next couple days, deaths are racking up in the tens of thousands, and both numbers are only headed upward from there.
In this post, I’ll try to game out what’s most likely to happen with the COVID-19 pandemic in the medium term — i.e. in the next month or two, the longest timescale on which we can even approximately foresee or even discuss specific events.
Note: This post uses three technical terms — R0, R, introgression — that are explained and illustrated in the last section, titled “Some background: key terms and concepts.” So if these terms are unfamiliar to you, head there first before scrolling back up to read the rest.
We also use concepts — i.e. Levels 1 through 5 — from our published framework for thinking through what’s next for COVID-19, and scenario descriptions from our scenario guide. Those are summarized in the last section below, as well.
What’s next: most of the first world will likely achieve control this spring
I’m going to make a contested and risky claim here, but I believe it’s very defensible and I’m pretty confident in it: most of the first world will not see uncontrolled spread to a majority of the population (Level 5 and a “big burn”) right now, but will contain their local epidemics and reduce the number of new cases in the next month or two.
This claim is risky because it goes against what a lot of knowledgeable people are saying; for example, the government of New York has projected that New York City will likely experience what we call a big burn, and during the first wave of this pandemic, no less. However, I believe I’m right.
The measures that we know can stop the epidemic, i.e., social distancing and widespread testing (see the next section), are not yet in place in many countries facing large outbreaks but are coming soon. The United States, for example, still has not gone to a general shelter in place order in half of its states, and still does not have testing capacity for contacts and mild cases. However, shelter in place orders are expanding, and on the testing front, test capacity is now up to over 65,000 tests per day, about half of what’s currently needed, and rising.

It’s also the case that drive-through testing centers are slowly emerging, and Abbott Labs will soon be rolling out tests that can be used in small clinics without specially trained technicians.
With governments and populations around the world increasingly aware that nothing but their success at containment stands between them and millions of deaths, and a set of clear examples available of how to achieve containment (see below), it’s not farfetched to suggest that they will ultimately do what is necessary.
In theory, any government ruling over a high-trust society with first-world medicine and sanitation, an organized police force, and enough biotechnology capacity to enable widespread testing should be able to contain their epidemic this spring. This is not to say that they all will, just that it’s likely many of them will, and that those areas who don’t have experienced a failure of government and political will, and not a wholly unavoidable natural disaster.
The bottom line: If you live in the first world, expect that your city may well see overwhelmed hospitals (Level 4) in April or May, but that it will likely also turn the tide during this timeframe. If your city sees a majority of its population infected this spring, it wasn’t unavoidable: blame the government and the public.
We now know how to contain the virus
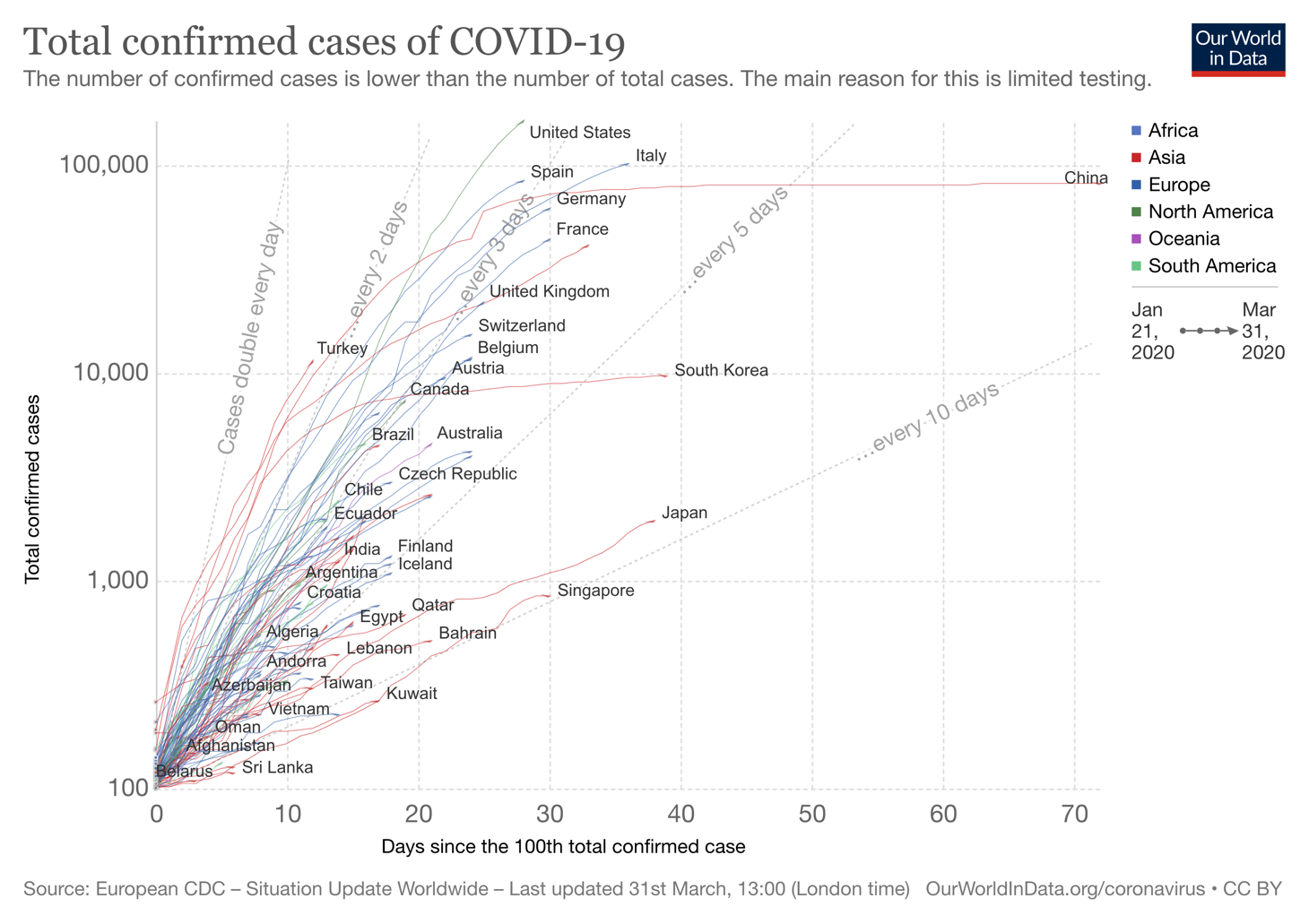
We know that many, many countries are achieving at least partial success in containing their local epidemics, a large number have cut its growth rate at least in half relative to R0, and at least a few have actually pushed R below 1 for a sustained period of time.
There are two things these success stories are using to control the spread of COVID-19:
- Social distancing, i.e. lockdowns and quarantines
- Widespread testing, so that we can identify who and where to focus on
China (outside Hubei) and South Korea have had the most success in using widespread testing and social distancing to combat COVID-19 — these countries have pushed R down to about .4, which is an eightfold drop from the disease’s natural R0 of about 3. These measures have been about as effective as similar measures were against SARS 17 years ago.
But in order to halt and then reverse the growth of a local epidemic, it’s not even necessary to be this successful; even reducing R half as much to about .8 will do the job.
There are other countries like Japan, Taiwan, Singapore and others that, while still facing local transmission, have kept their case growth down. Crude numbers suggest that these three countries, whose case numbers have all grown around eightfold in the last month, have kept their R-values around 1.5 over that period, and that’s including the impact of introgressions, so that the local R is somewhat lower. These countries, which are largely still running, are over halfway to containing the epidemic.
There’s also evidence that some degree of success in containing local epidemics is relatively widespread. Comparing total case numbers on March 29, March 23, and March 17, i.e. in the last two serial intervals of COVID-19 out of 253 jurisdictions in the Johns Hopkins CSSE coronavirus statistics database, which is the source of data for their widely used dashboard map, fully 175 of them had a lower percentage of growth in the second period than the first.
Even hard-hit countries like Italy, Switzerland, and Iran have managed to use lockdowns and quarantines to drop their growth rates to approximately the levels seen by Japan and Taiwan and Singapore over this time. And although neither Iran, Spain, or Singapore can say the same, new case numbers in Italy have been approximately flat for ten days, which suggests R may be even lower than this, perhaps as low as 1, already.
The bottom line: Social distancing and widespread testing are working for the countries that are doing them in a big way. To get this under control, we don’t even need to repeat the success of a South Korea — we can do half as well as they have and still get the case count down.
Which new countries and states will be hit harder in the next few weeks?
Local epidemics can sneak up on us. Italy, for example, went from only 3 confirmed cases to Level 4 in three weeks. However, it is possible to identify some countries and regions that seem to be in the process of moving toward a Level 4 local outbreak.
For example, if we apply a filter to the 253 regions in the CSSE dataset of having more than 1000 cases as of March 29 and a growth rate of over threefold in the prior six days (i.e. at or above the unconstrained rate of growth), while not currently having a Level 4 cluster, the following areas pop up: Quebec, Israel, the Philippines, Romania, Russia, South Africa, and Turkey. These could all be considered countries to watch in the coming week or two.
In the United States, data on the size and growth rate of the epidemic in different states seems to indicate that Washington and parts of New Jersey have some of the worst outbreaks outside New York, and unless they reverse trend will shortly follow New York into Level 4 status. Louisiana and Michigan are the most likely to follow shortly after that.
What happens comes after containment
So, COVID-19 has been contained, and we win, right?
Well, not really.
There are two realities preventing a return to normalcy once we get the outbreak under control:
- The kinds of intensive control measures that have successfully pushed R below one in other countries are not sustainable for long enough to truly eradicate the disease.
- Countries that achieve control in the next couple months will likely still be faced with a lot of introgressions from other countries with worse control of the epidemic.
The dynamic that countries will face after they contain the first wave of the COVID-19 pandemic has been described, in a widely circulated series of posts by Tomas Pueyo, as “the hammer and the dance.” While able to contain the epidemic with the “hammer” of shelter in place orders, governments will be unable to do this indefinitely and achieve eradication.
Governments will have to use granular feedback on the number of new cases coming from a saturation testing program to measure R in each area over time, and try to find a set of control measures, whether continuous or pulsed, that keep R less than one while allowing societies and economies to function viably (even if not ideally). These countries would still be subject to massive outbreaks relatively suddenly at any time due to superspreader events and other problems. This is referred to as the “dance.”
In the optimistic scenario, this might prove to be a relatively mild set of measures. It may be that saturation testing, along with massive public hygiene measures, can keep things from going out of control even as people begin going out again, or that economies retooled to have less interpersonal interaction can run with a lot less going-out than people thought.
Antibody tests to identify immune recovered patients, and vaccines arriving in small quantities, may make a critical difference by allowing immune people to be placed in what would otherwise be higher risk positions. Ramping up the protection of gloves, masks, and goggles, enough to allow the public to use them when out, will help too.
As these other factors improve and people and authorities become more skilled, the level of restrictions needed to keep R below 1 may get less stiff.
In a pessimistic scenario, no set of precautions allows many or most first-world areas to keep their R below 1 and their economy running simultaneously, so that there’s some combination of intermittent lockdowns and many months of elevated death rates and illnesses as the virus burns its way through the population.
There would also be some features of the pre-COVID-19 world that just wouldn’t come back, either for a very long time (e.g. large concerts and sporting events) or possibly ever (e.g. movie theaters and pants).
Potential game changers: medicine and the weather
In the long run, a large part of the progress of the pandemic will be determined by the many interventions that we can’t make now but will be enabled by advances in science, manufacturing, and logistics, including things like:
- Increasing supplies of masks, gloves, goggles, and so on, which would enable them to be more widely used by the general public
- New therapies which might help to make the disease milder or shorter for many people
- Vaccines, which could make those treated immune and help in a number of ways
- Increasing supply of ventilators to support serious cases
- Serological testing to identify which people had the disease in the past, which could improve epidemiological modeling, allow the economy to recover faster as immune people can take on higher-exposure positions, and reduce spread for the same reason
These interventions all have something in common: they’re not coming in quantity during the medium term.
The only measure other than simple social distancing that’s likely to have an effect in this timeframe is increased availability of PCR testing.
As for the change in the weather as the northern hemisphere enters the spring, much has been made of the possible impact of temperature on the virus’s transmissibility.
As we previously reported, while there’s no direct evidence, it’s seemed unlikely for a while that the temperature effect would be large enough to control the whole destiny of the pandemic. The evidence for this has continued to mount, as warm weather destinations like Brazil, Ecuador, Israel, California, Florida, and Malaysia, as well as southern hemisphere locales like Chile, South Africa, and Australia, have racked up thousands of cases each. While no Level 4 cluster has yet emerged in the southern hemisphere or tropics, this appears to be only a matter of time.
Some background: key terms and concepts
R0: The parameter that governs virus’s natural rate of growth, without any interventions. For a disease like COVID-19 with an R0 of three, each infected person typically infects three other people, and the serial interval, the average time between someone picking up the disease and passing it on, is about six days. This means the size of the outbreak will increase threefold every six days if we don’t do anything to slow it.
R: The parameter that describes the virus’s observed rate of growth in a particular area with a specific health system, set of social practices (mask wearing, hand hygiene, quarantines), and any other interventions that slow the spread. The goal of interventions is to get the R below 1, so that each infected person infects less than one other person and the outbreak begins to shrink.
Introgression: When some infections in a region are not the result of local transmission, but are rather imported into the region by infected people traveling into the region from outside it. Introgressions are a fancy term for “imported cases”.
Right now, the world record for reducing R in a real-world COVID-19 epidemic belongs to China and South Korea, both of whom have reduced R to approximately .4 in their Level 3 areas like Beijing and Seoul. This means that in these places, the number of new COVID-19 cases coming from local transmission (independent of imported cases from other places) is falling to about 40% of its prior value every 6 days. That is, in a month the number of new cases can fall by a factor of 100. This is how South Korea went from 800 new cases per day at the height of their outbreak’s growth to only about 100 cases per day only three weeks later.
But intermediate values really matter! For example, a place that reduces R from 3 to 1.5 by cutting half of transmissions can see its epidemic grow only eightfold in a month, even if it is still growing. And cutting R to .8, while it won’t allow a South Korea style collapse in case numbers, will prevent the epidemic from growing out of control and allow it to slowly shrink over time, approximately threefold per month.
In our published framework we divided up degrees transmission of the virus into levels, described as follows:
- Level 0: There are no active cases of COVID-19 in a given area. The default state of things.
- Level 1: There are some active cases of COVID-19, but they are all contained. Unless this containment is broken or more cases arrive, reversion to Level 0 will follow shortly.
- Level 2: There is local transmission of COVID-19, but it is small. If all the cases were known, they could e.g. be separated into clusters with some degree of accuracy.
- Level 3: There is widespread local transmission, e.g. enough to thwart cluster tracking even with good effort, but the disease burden is low enough that medical facilities are not overwhelmed.
- Level 4: The local disease burden is large enough to overwhelm medical facilities, but still small relative to the local population as a whole.
- Level 5: The local disease burden is large enough to make up a significant fraction of the local population.
Our scenario guide outlined three scenarios that are referenced in the current post:
- Scenario 1: Containment and Eradication — this is the most optimistic scenario, where we contain the outbreaks long enough for effective therapies to come along and let us eradicate it.
- Scenario 2: Sideways until Therapies — our intermediate and most likely scenario, where things get pretty bad in specific cities and countries until we get effective therapies to help us control it.
- Scenario 3: The Big Burn — the worst-case scenario, where the virus spreads largely uncontrolled through the bulk of the population.



You are reporting the comment """ by on