For months, we’ve been saying that SARS-CoV-2, the virus that causes COVID-19, can survive on surfaces—even when the CDC appeared to be saying the opposite. We’ve also written about how asymptomatic cases are probably underestimated. At this point, we’re preaching to the choir.
But this afternoon, a new study was published in mSphere, and it examines something that hasn’t been widely studied: just how do COVID-19 patients contaminate their surroundings? And where do they spread the virus?
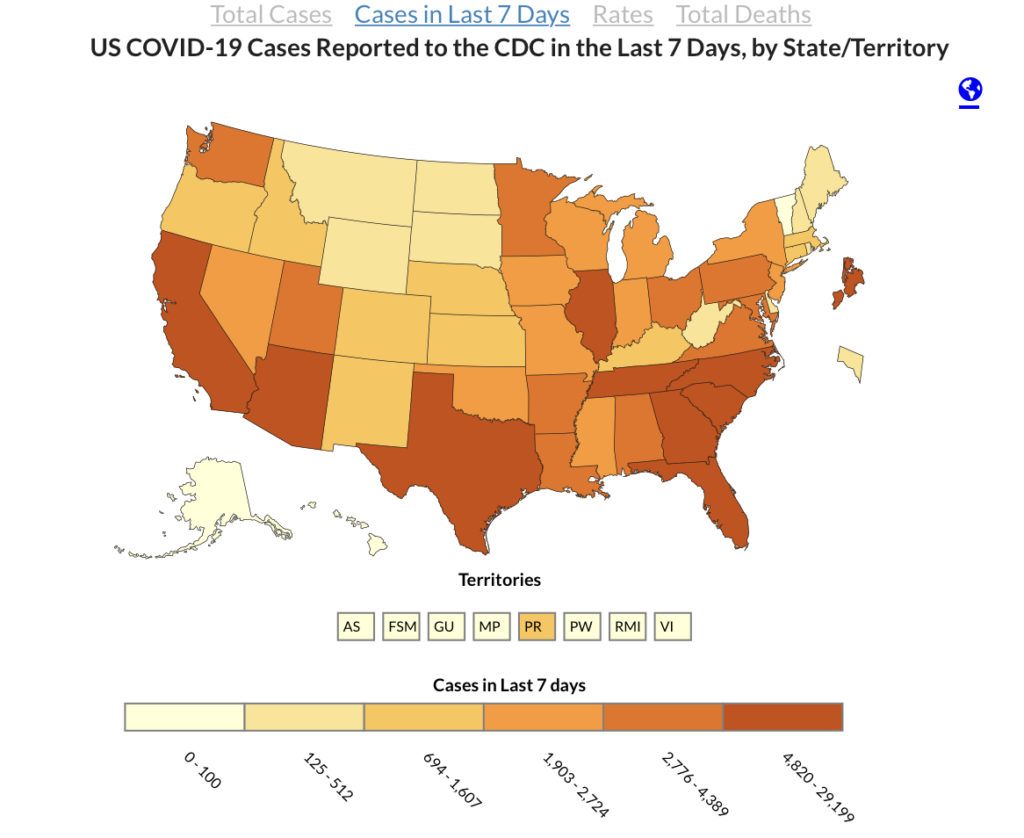
Importantly, the study shows that both symptomatic and asymptomatic COVID-19 patients can contaminate their surroundings. Intellectually, these findings make sense. Of course it’s not just those who are in the hospital or feeling really sick who can spread the virus. But the study mentions a ‘false feeling of safety’ that rings true as we watch the new cases map turn red again even as bars and restaurants reopen.
Here’s what you need to know:
- Surfaces are very risky! Polymerase chain reaction (PCR) testing revealed the 39.3% of surface samples were positive for SARS-CoV-2. But in some hospital rooms, more than 90% of surfaces were positive for live virus.
- All of the air samples were negative! That means you can breathe easily in an empty room—as long as you don’t touch anything at all. It’s still vitally important to wear a mask.
- The study suggests that it might not be possible for asymptomatic COVID-19 patients to self-isolate at home. Shelter hospitals, like the ones used in China, might be a better way to go.
How the study worked
Researchers in Chengdu, China sampled the surroundings and air in the hospital rooms of 13 COVID-19 patients. Eleven patients had symptoms, but two of them tested positive despite having no symptoms. The patients had returned from overseas and were placed in isolation wards after testing positive. Their rooms had negative pressure, which is what hospitals typically use to make sure air can circulate within a room but can’t get out.
On April 2, researchers took samples from air and objects in the patients’ rooms, including: bedrails, room and toilet door handles, light switches, foot flush buttons, sink rims, sink and toilet bowls and drains, bedside tables, bedsheets, pillows, equipment belts on wall, floor, air exhaust outlets and the air itself.
The objects in the room were, as the researchers put it, “extensively contaminated.” Of the 112 surface samples the researchers collected, 44 of them tested positive for SARS-Cov-2. That’s 39.3% of objects around the room.
In some rooms, 4.6% of the tested objects were positive for SARS-CoV-2. In other rooms, 95.7% of the objects tested positive. The top five contaminated sites:
- Bedrails (53.9%)
- Pillows (50%)
- Bedsheets (50%)
- Air exhaust outlets (50%)
- Light switches (40%)
It wasn’t that the rooms hadn’t been cleaned. Nurses disinfected the rooms and toilets twice a day with 2,000 mg/L chlorine solution. Researchers took the samples 4-7 hours after they’d been cleaned for the first time that day.
“In a single room with an asymptomatic patient, [four] sites including bedrail, pillow, bedsheet and the air exhaust outlet were SARS-CoV-2 positive,” wrote Dr. Zhiyong Zong, MBBS, PhD, and colleagues. “This highlights that asymptomatic COVID-19 patients can contaminate their surroundings and therefore make persons who have direct contact with them such as their family members and healthcare workers be exposed to SARS-CoV-2.”
Less aerosols, more droplets
We know that COVID-19 is mostly passed from person to person, and you’re at the greatest risk for contracting the disease if you spend extensive time sharing space with an infected person. But in this study, all of the air samples in the study tested negative for SARS-CoV-2.
For this study, researchers took samples of the air during routine late-morning activities. They sampled the air for 15 minutes from 0.6 m away from the COVID-19 patient. All of those samples were negative for SARS-CoV-2. Meaning: breathing in the air around an infected person wasn’t as risky as touching their bed.
Still, half of the air exhaust outlets in the rooms tested positive. And in the rooms with positive air exhaust outlets, many more surfaces were contaminated. Researchers think this means that small virus particles could be carried through the air from these exhaust outlets and scattered around the room.
So while the study found less positive aerosolized virus particles, it found that droplets of the virus traveled through the air and settled all over surfaces. Coronavirus particles could still be blowing through the air to land on surfaces. And someone talking to you could still exhale particles that could make you sick. So it’s extremely important to wear a mask.
The researchers added a big caveat to their study’s conclusion: “Although we collected 1,500 liters of air for each air sample, that amount represents a low volume compared to the whole space of the room. We tested only for viral nucleic acid and did not perform viral culture to test viability.” Basically, their study isn’t conclusive when it comes to air and SARS-CoV-2. We have to do a lot more research to understand how the virus lives in the air.
Also important: this study was conducted in the hospital setting. We still don’t know exactly how particles travel through the air in homes, stores, and outside.
This study doesn’t change the idea that we should wear masks when around other people who could sneeze, cough, or laugh on us. But after other people leave the room, you’re unlikely to catch the coronavirus from the air you breathe. Instead, you should pay extra attention to all of the surfaces you touch. The virus may have passed through the air and landed on plenty of surfaces.
More on mask advice:
- Smooth operator: the compleat gentleman’s guide to beards, masks, & pandemic shaving
- You can use an old prom dress to make a mask that works like an N95
- Review: the GORUCK face mask
- How to safely put on and remove personal protective equipment like masks & gloves
Surface contamination is high
The study showed that surface contamination is high, and we should be extensively cleaning shared surfaces. Between disinfecting with the chlorine solution and taking the test swabs, surfaces were contaminated in just a few hours.
The bottom line: cleaning a surface doesn’t mean it’s disinfected for long. So even though grocery store workers are constantly disinfecting shopping carts, baskets, and aisles, virus particles could settle on them right after they’ve been cleaned. Even an asymptomatic person in a recently-cleaned public bathroom could contaminate the door handle, light switch, toilet seat, and sink.
When you come in contact with a surface outside of your home, clean your hands and don’t touch your face!
The worst news is for households where some people have been relaxing their social distancing measures or taking fewer cleaning precautions. The study suggests that an asymptomatic or pre-symptomatic family member could contaminate every surface in the home before anyone realizes they have COVID-19. That’s why the researchers are suspicious of at-home isolation. Coronavirus particles could get in the air conditioning, in the vents, and all over surfaces even after you’ve cleaned thoroughly.
The best way to go: stay home as much as possible, clean everything you touch, wear a mask whenever in public, and thoroughly sanitize yourself and your surroundings as often as you can.


You are reporting the comment """ by on