Liu Zheng Zheng of the Harvard Business Review China, based in Beijing, contributed to this report
Last updated: 01-27-2020 at 3:00 pm ET
A previously undiscovered respiratory virus originating in Wuhan, Hubei province, China has given rise to a rapidly growing, headline-grabbing viral epidemic that’s now spreading across the world as we all watch the news reports in real-time. This novel coronavirus virus goes by the names “Wuhan Pneumonia” and 2019-nCoV, and while it has not yet officially been declared a “Public Health Emergency of International Concern” by the World Health Organization, it is serious enough to keep a close eye on.
We’ll continue coverage of this outbreak so you can cut through the fear and panic noise.
Fast facts (updated as we know more):
- There is cause for alarm, but it’s not time to panic. Keep in mind that normal flu kills around 40-60,000 people per year in the US.
- There remains considerable uncertainty about where the virus has spread and the real case numbers.
- The virus is spread mainly through droplets in the air (eg. when people exhale/sneeze/cough), mainly infects the lungs, and causes symptoms, like fever, fatigue, a dry cough, and respiratory distress. It can spread from patients who do not exhibit symptoms, but it’s unclear how often this happens.
- This could get very bad, but it won’t be doomsday. For many reasons detailed below, the 1918 Spanish Flu outbreak looks like a solid upper limit on how bad things could get with this virus in terms of impact on society. As bad as the Spanish Flu was, modern infrastructure still ran, the grocery stores were still stocked, the stock market still traded, and in general life went on.
- This epidemic’s progress has been rapid, and the current status is large, widespread, not contained, and growing quickly. It appears to have entered a phase of rapid exponential growth and geographic spread.
- The Wuhan strain appears to have about the same incubation period as SARS, possibly a bit shorter, in the range 5-10 days. This is is contrary to early reports indicating a longer two-week cycle.
- The reproductive number of the outbreak is uncertain, but responsible estimates have ranged between 1.4 and 4. This number, explained in more detail near the end of this article, needs to get below one for the outbreak to shrink.
- Most cases appear to involve transmission between people with some direct connection to each other, like family members, coworkers, and patients communicating the disease to medical staff in hospitals.
- Transmission between unrelated people in public spaces appears to be rare, although there is considerable uncertainty about this.
- The case fatality rate (CFR) of the Wuhan coronavirus appears to be qualitatively higher than influenza and much lower than something like Ebola or untreated HIV, but could be lower than SARS (<10%), and very likely lower than MERS (40%).
- It is possible that existing antiviral drugs could be repurposed against the Wuhan coronavirus, but unlikely that new therapies will emerge on the timeline of an epidemic like this.
- It’s unlikely that the lockdown measures inside China will stop the virus’s spread from city to city, but it is entirely possible that quarantine measures can stop the spread of the virus inside cities once it gets to them. We’re missing too much information to justify either pessimism or optimism on any of these points right now, though.
About the author: I am a biomedical scientist with a Ph.D. in computational medicine, and I develop lifesaving medicines for a living. I am not a physician or a virologist, but am able to parse all of the data floating around.
Latest updates:
- [01-27-2020, 10:03 pm] The confirmed case number is now over 4,500, including over 2700 cases in Wuhan, over 100 in six other Chinese cities, and 65 cases in 18 countries/territories outside China. Known human-human transmission outside China is still very limited. Deaths have risen to over a hundred. Case numbers are still doubling every two days, and several days remain until we have even an early indication of the effectiveness of the quarantine.
- [01-27-2020, 8:14 pm] Report from Beijing: life during the Wuhan coronavirus outbreak
- [01-27-2020, 1:30 pm] General updates: the media coverage gets darker, but there’s good news.
- [01-27-2020, 11:30 am] Why this Wuhan case, and the Chinese gov’s fast and large lockdown in response, is likely the new normal in modern countries.
- [01-25-2020, 10:53 pm] The latest clinical reports and results of academic epidemiological models are at odds with what US public health authorities have been telling the public.
- [01-25-2020, 9:42 pm] Our full report on the latest developments.
- [01-25-2020, 9:42 pm] Our in-depth analysis of four academic models of the spread of the disease.
- [01-25-2020, 8:43 pm] The South China Morning Post is reporting case numbers over 2,000 total cases, with a larger but unknown number of infections among healthcare workers.
- [01-25-2020, 7:44 pm] Here’s our more detailed post dedicated to the latest news on the Wuhan virus, with discussion of its origins, the latest out of China itself, global spread, and trying to nail down key epidemiological parameters.
- [01-25-2020, 6:46 pm] We published a piece debunking the widely spread notion that the Wuhan virus is some sort of escaped bioweapon. It almost certainly is not.
- [01-25-2020, 2:57 pm] Genetic studies have confirmed that the 2019-nCoV strain originated in bats before traveling to humans through an animal intermediary.
- [01-25-2020, 2:57 pm] The CDC has evaluated as many as 63 potential cases in the USA, but so far the two cases in Seattle and Chicago remain the only two confirmed cases.
- [01-25-2020, 2:57 pm] The epidemic in Wuhan continues to escalate with over 1400 cases, as China has put over 46 million people under lockdown, banned private vehicle travel, sent over 1200 medics, and is building a second hospital, while the USA has announced it will evacuate US citizens by private jet.
- [01-25-2020, 2:57 pm] Elsewhere in China, intercity buses and trains have been shut down in Beijing, and closures of public places including schools, monuments, theaters, and public celebrations have been seen nationwide. Chairman Xi described the situation as “grave.”
- [01-25-2020, 2:57 pm] Major disagreement among scientists over the virus’s epidemiological properties continues, with no emerging consensus on the virus’s reproductive number or latency period.
- [01-24-2020, 5:49 pm] There are now 1125 confirmed cases and 41 deaths so far. Of these the vast majority were in Hubei province and only a handful were outside China. However, thousands of unconfirmed cases are currently backlogged in Wuhan’s overwhelmed hospitals, and case numbers have been growing exponentially day by day.
- [01-24-2020, 5:49 pm] There are only two confirmed cases in the United States, one in Seattle and one in Chicago. There are suspected cases in Texas, Los Angeles, and Michigan, and possibly other places.
- [01-24-2020, 5:49 pm] The very first known case of human-human transmission outside China was confirmed today.
Be prepared. Don’t be a victim.
Want more great content and giveaways? Sign up for The Prepared’s free newsletter and get the best prepping content straight to your inbox. 1-2 emails a month, 0% spam.
What is the Wuhan coronavirus?
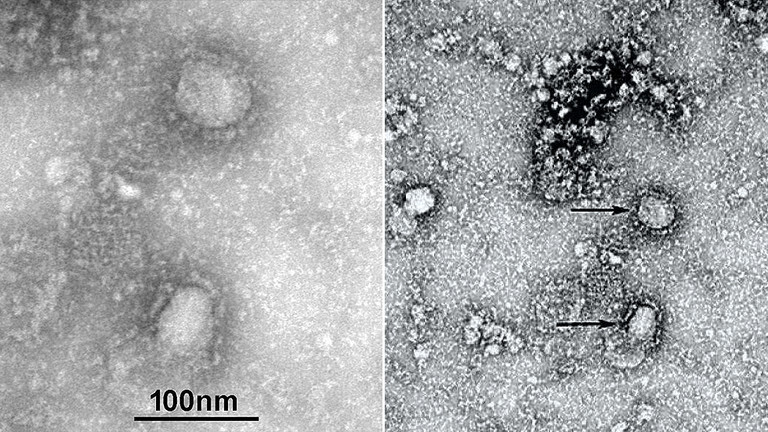
The Wuhan coronavirus is a newly discovered seventh type of human coronavirus, which is causing the ongoing epidemic in Wuhan, other parts of China, and a growing number of other countries around the world.
Coronaviruses are one of the two families of viruses that infectious disease experts expect the world’s next major pandemic to emerge from. (The other being influenza viruses.) The SARS epidemic of 2002 and the MERS epidemic of 2012 were both coronaviruses that we initially feared might result in a global pandemic, before they were contained.
How bad could this coronavirus outbreak get?
In theory, very bad, but even if it’s as bad as the 1918 Spanish Flu it won’t be anything like the end of civilization.
It’s difficult to estimate the number of people a rapidly spreading respiratory virus could infect in the modern world, but the hardest we were ever hit by such a virus was the 1918 influenza pandemic. The so-called Spanish Flu is estimated to have hit 30% of the global population and had a case fatality rate of 10% to 20% — on the same order as current estimates for the Wuhan coronavirus. This pandemic overwhelmed all medical facilities around the world, and killed between 3% and 6% of all living humans.
With the state of medicine so much more advanced than it was a century ago, it is difficult to imagine that the Wuhan coronavirus could do worse than this, even in the worst-case scenario.
The two viruses, although genetically different, are somewhat similar in some of the main properties that govern the spread of an outbreak. The 1918 Spanish Flu virus had a latency period between 2 and 7 days, which overlaps current estimates of the Wuhan coronavirus’s latency period. Its base reproduction number in different settings ranged from only 1.2 (in a good hospital) all the way up to 7.5 (among family members in a confined space), on the same general order as estimates for the Wuhan coronavirus.
Both Spanish Flu and the Wuhan coronavirus are droplet-spread respiratory viruses, with significant overlap in symptoms. And while most warnings about “the next global pandemic” make much of the modern world’s interconnectedness, the Spanish Flu did make it nearly everywhere in the world and infect 30% of the global population, so a global pandemic is already a known event in history.
History provides a good record of what happened in the Spanish Flu. Governments stayed intact, the utilities stayed on, and there was food in the grocery store. Society kept functioning even as people got sick and died. In the very unlikely event that the Wuhan coronavirus somehow became a global pandemic, this would very likely continue to be the case.
So there is little reason to think that the Wuhan strain can do anything the Spanish flu couldn’t. Accordingly, it probably makes little sense to prepare a total breakdown of society — even when gaming out the very worst possible scenario.
Much more likely, however, is that public health measures, medical science, and humans coordinating our actions will contain the epidemic, and a year from now this section of this article will look like the irresponsible speculation that it almost certainly is.
How accurate is our information about the virus’s origin, genetics, biology, and epidemiology?
[Updated January 27, 9:42 pm]Not very accurate. We have enough info so far to get roughly in the ballpark on some of the key factors that define the spread and severity of an outbreak, but we won’t be able to nail those numbers down for a few more weeks.
While the virus’s origin was initially obscure, some clarity has emerged in the last week. Sequencing of the viral genome has revealed that it came from bats, probably by way of an unknown intermediary, and among human coronaviruses is most closely related to SARS. We’re very sure that the virus moved from animals to humans in a particular area of the seafood market in Wuhan and that it is not an escaped bioweapon.
The virus’s genome has been sequenced reliably, and over two dozen different viral genomes are available from different patients, enabling early phylogenetic work to begin. Ongoing study will be needed to further understand its origin, relationship to other coronaviruses, and the effect of its unique properties on the disease’s behavior in humans.
Our current estimates of the virus’ latency period, incubation period, basic reproductive number, and case fatality can get us in the ballpark as far as estimating the virus’ possible impacts, but we need to nail down those numbers further in the next few weeks to get a clearer picture of how bad this is or could get. Experts have been citing incubation period numbers from 3 to 10 days, and basic reproductive numbers as low as 1.4 and as high as 4.0. In particular, we have no real idea of the longer term effects of being infected with Wuhan coronavirus.
What has been the progress of the current epidemic, and what is its current status?
[Updated January 27, 9:42 pm]The epidemic’s progress has been rapid, and the current status is large, widespread, not contained, and growing quickly.
Wikipedia’s chronology article has the best summary I’ve been able to find in any one place, and is updated rapidly.
While the first symptoms were observed on about December 8, the case didn’t come to the attention of health authorities as a cluster of related cases until December 30. On December 31, the seafood market was identified as the origin point, and the first precautions were taken. The seafood market was closed on January 1. Neighboring countries began to take travel precautions.
By January 5, SARS, MERS, and the flu had been ruled out, and a novel coronavirus was confirmed on January 9. The virus’s genome was sequenced the very next day.
By January 10, the epidemic, though real, could be treated as a curiosity. Although there were 41 cases and it was known that a novel virus was responsible, the cases all had direct contact to the origin point and there was no direct confirmation of human-to-human contact. In addition, all the cases were located in Wuhan, and no new cases had been reported in five days.
On January 13, the first case in Thailand emerged, and on January 14, a case in Wuhan emerged that suggested human-to-human transmission. The first laboratory test to confirm cases of the disease was released on January 15. Thailand reported a second case on January 17, and the United States implemented fever screening for direct flights arriving in the USA from Wuhan on this date.
It was at this point that the epidemic began to escalate much more rapidly. On January 18, China reported the number of cases had escalated to 62, and on the 19th, to 201, including cases outside Wuhan. It’s unclear how many of these cases had actually emerged in this time period, and how many emerged earlier and merely escaped detection. It was at this point that the epidemic began to worry me.
On January 20, additional cases were confirmed in Shanghai, Beijing, and Guangdong, and the first cases in South Korea. It was also definitively confirmed for the first time that the disease had spread from humans to humans.
On January 21, Wuhan reported over a hundred additional cases, bringing the total to 320, including 15 cases among medical staff who had been using droplet precautions. In addition, cases were first reported in an additional nine Chinese provinces plus Taiwan and the United States.
This last case, the first confirmed in the USA (there is a second case as of this writing), was a man who arrived in the USA from Wuhan prior to the initiation of travel precautions on September 17. It remains unclear whether the precautions would have allowed his case to be detected on entry, whether he infected anyone before being hospitalized, whether he will infect anyone in the hospital, and whether additional infected persons have entered the USA from Wuhan or elsewhere.
The epidemic appears to have entered a phase of rapid exponential growth and geographic spread. As of [01-27-2020, 9:45 pm], the number of confirmed cases is over 4,500, with 106 reported deaths, and the number of confirmed cases continues to double about every two days. Human-human transmission has been reported in Vietnam and Thailand, but no first world country.
While most cases are in Wuhan, almost every province in China has some cases, and cases have been reported in eighteen countries and territories outside China. The United States currently has five confirmed cases, in Seattle, Chicago, Los Angeles, Orange County CA, and Arizona, with the CDC evaluating over 100 more. All US cases came from Wuhan, and there is still no evidence of transmission inside the USA.
What’s likely to happen in the near future?
[Updated January 27, 9:42 pm]A lot of things, all at once. Specifically many more confirmed cases in many more places will pop up, both in the US and in other countries. The WHO may revisit its decision not to declare a public health emergency. And we’ll get more clarity in the key parameters and viral properties that define the outbreak, as well as on how well our measures to contain it are working.
The number of diagnosed cases of this disease is all but certain to continue growing rapidly into the thousands. Because the incubation period of the disease appears to be as long as ten days, cases being diagnosed today were first infected around January 17, before significant measures had been taken to halt the spread.
It will be another week at least before we know about all the additional cases which entered the USA before the precautions (if any), and another two weeks before we’ll know how much the lockdown in Wuhan has reduced the rate of spread.
Numerical predictions of how much the case count could grow in this period are impossible to offer with any degree of precision, but the number of known cases has expanded tenfold since January 18, and it is quite possible that a similar expansion will occur before we even have the chance to see the effects of recently instituted protective measures. However, growth rate estimates are notoriously difficult to quantify in the early stages of epidemics due to the tendency for old cases to be discovered later, which can either reduce or inflate estimates based on case numbers over time. And in addition, the growth rate may have changed.
It is virtually certain that more cases of the disease will be confirmed in the USA and other countries, for the same reason.
It is quite possible that as this information emerges, the WHO will soon revisit its decision not to designate a Public Health Emergency of International Concern in Wuhan.
As time passes, our estimates of the epidemiological parameters of the disease will tighten. More constrained estimates of the latency period, basic reproduction number, and case fatality rate should be available within a few weeks. In addition, the symptom profile of the disease and optimal supportive care measures will be better understood.
Finally, and crucially, we will begin to be able to see how effective China’s massive quarantine and lockdown, and measures taken in other countries, are at preventing spread inside hospitals and in countries where the epidemic has just landed.
Are there any drugs that work on this coronavirus?
None are known, nor are any likely to be developed before this outbreak runs its course.
No antiviral therapies are currently known to be effective against the Wuhan coronavirus, and we have not been able to find any reports of clinical research in this vein.
Laboratories with experimental coronavirus therapies in both industry and academia are surely working as fast as they can to identify whether their therapies could work against the Wuhan strain. This could involve a painstaking process of building homology models of viral proteins on the basis of the published viral genome and then performing molecular docking calculations to see if drugs directed against other coronaviruses will function with the Wuhan strain, or rushed biological experiments, undertaken in highly secure virology labs, to determine the same thing. It would also involve rushed work on logistical and regulatory fronts to determine whether the therapies are ready to try in the clinic.
During the 2014 Ebola outbreak, these approaches achieved some highly notable successes, which led to both a treatment and an effective vaccine, but coronavirus outbreaks move so much faster than Ebola outbreaks that it’s unclear if they will yield any results in time.
So the efforts to treat the Wuhan virus in the field will likely be limited to just helping victims cope with symptoms, at least for the foreseeable future.
Can we develop new drugs against this coronavirus? How about a vaccine? How fast?
It’s possible that existing antiviral drugs could be repurposed against the Wuhan coronavirus, but unlikely that new therapies will emerge on the timeline of an epidemic like this.
As discussed above, laboratories around the world are working around the clock to evaluate existing antiviral drugs, particularly experimental coronavirus therapies, for their potential against the Wuhan strain in light of the virus’s recently sequenced genome. Time will tell whether any significant hits emerge, whether they can be translated into clinical trials, and what success, if any, such trials show.
However, it’s unlikely any new therapies can be developed within the timeframe of this outbreak. Even relatively rapid-to-develop therapies like antibodies and therapeutic nucleic acids usually take months just to prototype, and months more to qualify, and months more to scale up, and typically years to translate to the clinic. Past coronavirus outbreaks have been eradicated in less time than it would take to go through this long therapy development process.
There have been some reports that an RNA vaccine may be ready for a preliminary trial in a matter of months, but this timeline is highly uncertain.
What can people who think they may have the Wuhan coronavirus do?
If you think you may be infected, immediately put on a surgical mask and get to the nearest hospital. Present yourself for treatment and monitoring, and tell the physicians and scientists everything you know about where you’ve been and who you’ve been in touch with.
What can people in an affected area do?
- Don’t panic.
- Wash your hands regularly with soap and water, and don’t touch your mucous membranes with unwashed hands (eyes, nose, mouth).
- If you want to, wear a respirator in public. Remember that basic surgical masks don’t protect you from other people, they protect other people from you.
- Limit social interaction and time spent in public.
More: Read the beginner’s guide to and our reviews of the best respirators
What can people in an unaffected area do?
Relax and read the news to see if events change. Consider what you would do if your area became affected.
Have you followed the beginner’s checklist to have at least two weeks of supplies in your home so you can avoid other people if you need to? Do you have respirators?
What key pieces of information should we be looking for in future press coverage to determine how worried to get?
As estimates firm up of the epidemiological properties of the virus, and the ability of various measures to contain it, we will know how bad it’s likely to get.
Specifically, the following numbers will tell us what we’re in for:
- case fatality rate
- latent period
- incubation period
- basic reproduction number
We’ll also keep an eye out for answers to the following questions:
- Is the lockdown in Hubei province sufficient to arrest the growth of the epidemic? (We likely won’t know for a few weeks.)
- Can we prevent doctors and nurses from getting infected inside the thousands of beds worth of coronavirus wards now being set up in Hubei?
- Do other cities in China succeed in containing the spread of their cases, or do local epidemics like Hubei establish themselves in other cities?
- Do new cases of the coronavirus stop arriving in countries outside China in the coming weeks, or do they continue?
- Does human-human transmission begin occurring in meaningful numbers outside China?
Just as important as knowing what to pay attention to is knowing what to ignore, because certain pieces of information that sound bad may reveal relatively little.
For example, if cases of the virus are detected in thirty countries in the next week, or the case numbers in Hubei grow fiftyfold over the next two weeks, this may simply show the delayed effects of epidemic growth before protective measures were put in place. So what we really want to know is whether those measures are effective once their effectiveness becomes measurable, some weeks from now.
The press and the public have a tendency to lurch between unawareness and blind panic. Please, don’t. Read carefully and think, but don’t read too much into scary points. Keep your eye on biological, medical, epidemiological and social fundamentals.
What are the Chinese authorities doing to stop this?
[Updated January 27, 9:42 pm]A great deal, including putting over 46 million people in quarantine as of [01-25-2020, 2:57 pm], building a new hospital in a matter of days, limiting the size of public gatherings, screening travelers, closing public venues like movie theaters, and having people stay indoors as much as possible.
In Wuhan and its surroundings, the government on January 22 announced that it would halt all trains and flights out of Wuhan effective on the morning of January 23, and stop all public transit within the city at the same time. This was expanded the next day to include a recommendation that Wuhan residents stay in their homes except as necessary, and a ban on leaving Wuhan except by special permission.
Bridges and ferries allowing travel between the city’s three districts were also closed to all non-official traffic.
Later that day, the quarantine and lockdown were progressively expanded to additional cities near Wuhan, including Huanggang, Ezhou, Chibi, and Zhijang. A quarantine order for Xianning, Xiantao, and Zhijiang will go into effect on the morning of January 24, and further areas of Hubei were added on the evening of January 24. This will put a total of about 35 million people under lockdown. So far, these measures are confined to the immediate surroundings of Wuhan, and all within Hubei province.
In addition, there is an effort to deliver more physicians and supplies to expand capacity to care for the sick in Wuhan, including more virology laboratory capacity. The Chinese government has announced that it is declaring special wards for coronavirus in Wuhan with a capacity of 2,000 beds and building a dedicated field hospital with a capacity of over 1,000 beds using prefabricated structures.
So far the number of confirmed patients doesn’t seem to have exceeded existing hospital capacities, let alone these expanded numbers. However, long queues of patients seeking to be evaluated have reported, and over 8,000 patients in Wuhan and the surrounding areas are currently being evaluated for the coronavirus.
Elsewhere in China, travelers are being screened with infrared thermometry, and those found to have fever are being evaluated for the Wuhan coronavirus. People have been encouraged to limit travel despite the upcoming Chinese new year travel season. Large public events like new year celebrations have been canceled, and densely trafficked places like Beijing’s forbidden city, Shanghai’s Disneyland, and the country’s 70,000 movie theaters have been closed even in unaffected areas.
Liu Zheng Zheng has given The Prepared an in-depth first hand report from Beijing.
What is the international community doing to stop this?
The WHO and virological experts are coordinating extensively, and researchers are working around the clock to understand the virus’s genome and figure out whether any existing therapies could be repurposed to fight it.
There is also an ongoing effort to expand the availability of diagnostic testing to detect the virus.
So far, none of this appears to have translated into clinics in Wuhan, and the city is not generally considered to be in need of an Médecins Sans Frontières (MSF) presence in the same way as third world countries without widespread access to modern medicine.
The WHO announced on January 21 it would hold an emergency meeting the next day to determine whether the outbreak constituted a Public Health Emergency of International Concern (PHEIC). On January 22 and again on January 23, WHO leaders met, but on both days decided not to declare such an emergency. They have announced they will convene another meeting within ten days.
And of course, countries around the world are instituting checks for travelers from the affected regions, and isolating and treating the cases they do identify.
How accurate is our information about the epidemic’s progress?
Potentially not very accurate, particularly on the margin. There’s still a lot of uncertainty about where the virus has spread and the real case numbers.
For example, as of this writing, Hong Kong has over 140 cases of suspected Wuhan coronavirus, including 60 which predate January 10. If a significant portion are confirmed, the Hong Kong outbreak could come close to rivaling the Wuhan outbreak in size. However, Hong Kong still has only two confirmed cases, and no English-language reports have yet revealed testing results on the mass of suspected cases, which may not have been carried out yet due to the limited number of laboratories capable of administering the tests.
In addition, some of the lockdown and quarantine measures taken in Wuhan have been extended to nearby cities which have few or no confirmed cases in English language reports. It’s unclear whether many more cases are expected in these areas.
Finally, with an incubation period of up to two weeks, the cases we have seen reported in the last few days were infected two weeks ago, and the number and location of people infected since then who are not yet reporting symptoms remains a very large unknown.
How can we tell if a sick person has the Wuhan coronavirus?
People are being rapidly screened by checking for fever, which is the most universal symptom of the disease. Those with matching symptom profiles and a history plausibly connecting them to the epidemic (eg. having come from Wuhan or being connected to someone who has) are subjected to additional testing measures. This may include x-ray imaging of the lungs to detect the characteristic abnormalities of a coronavirus infection.
However, the most reliable tests for Wuhan coronavirus specifically are the ELISA test, which looks for Wuhan coronavirus proteins in the blood, and the PCR test, which looks for unique sequences from the virus’s genome which differentiate it from any other viruses.
Both of these tests have been rapidly developed and deployed by coronavirus researchers in response to this epidemic in recent weeks. Patients who test positive on either of these tests are referred to as laboratory-confirmed, and this count is considered the most reliable way to evaluate the size of the epidemic.
Where did the Wuhan coronavirus originally come from?
[Updated January 27, 9:42 pm]The virus first spread to humans in early December 2019, in the Huanan Seafood Market in Wuhan, the capital of Hubei Province, China. This market, similar to the origin point of the SARS epidemic, sells a wide variety of animals for food, including wild and exotic animals, and by all accounts enjoys poor sanitary conditions.
The first cases were concentrated among the workers and customers of a small number of nearby stalls, and genetic study has revealed that bats were the original host organism, but it remains unclear which animals were the intermediary. It is not a bioweapon.
Initially there was discussion of civet cats as an intermediary, similar to the SARS epidemic. However, other research has investigated badgers, bamboo rats, and direct transmission from horseshoe bats. These conclusions may change over time.
What properties does the new coronavirus have relative to other viral illnesses and other coronaviruses, and how sure are we about these things?
[Updated January 27, 9:42 pm]Both medically and genetically, the Wuhan coronavirus appears most similar to the SARS coronavirus. Although its genome is only about 70% identical at the RNA level, the proteins appear to be much more related, particularly important proteins related to the virus’s recognition and attack of its host cells.
The virus is spread mainly through droplets in the air, primarily infects the lungs, and causes a similar battery of symptoms to SARS, like fever, fatigue, a dry cough, and respiratory distress.
In terms of key epidemiological parameters, expert estimates on the latency period and incubation period vary significantly, but the incubation period appears to be shorter than initial estimates of two weeks, and asymptomatic transmission has been seen in some cases (but how often this really happens remains to be seen). The length of the latency period is less clear, and may be as short as SARs at 4-6 days. It has been confirmed that in the time since the first symptoms emerged, the virus has passed through at least three generations of humans in some cases.
The reproductive number of the outbreak is correspondingly uncertain, but responsible estimates have ranged between 1.4 and 4. We’ve done an in-depth comparative analysis of academic models of the virus’s spread. Most cases appear to involve transmission between people with some direct connection to each other, like family members, coworkers, and patients communicating the disease to medical staff in hospitals. Communication between unrelated people in public spaces appears to be rare, although there is considerable uncertainty about this.
The Wuhan coronavirus appears to have a case fatality rate qualitatively similar to SARS and MERS, but with a great deal of uncertainty about this number. As of this writing, 106 deaths have been observed, while the number of cases reported was only 291 a week ago. This and similar analyses have led fatality estimates as high as 40% to circulate among laypeople. However, experts stress that this kind of estimate is not reliable, and fatality rates are often overestimated early in an epidemic.
So, for now, we can say that the case fatality rate of the Wuhan coronavirus appears to be qualitatively higher than, say, endemic influenza, and much lower than something like Ebola or untreated HIV, but could be anywhere from 1% to higher than SARS at 10%.
What have scientists done so far to learn about this virus and stop it?
[Updated January 27, 9:42 pm]Researchers have sequenced the virus’s genome and are analyzing it. Epidemiological models are being fit to the available data to predict the virus’s spread.
All the available clinical data is being pooled and analyzed by virology experts, with updates going out to the treating hospitals as available.
And of course effort is being expended by labs around the world to look at opportunities to repurpose available antiviral drugs against the Wuhan strain.
How effective will the Wuhan lockdown be at limiting the spread of cases inside Wuhan?
Probably pretty effective, but the answer is far from certain.
As discussed above, it’s very likely that thousands of cases are already latent inside Wuhan, and any such estimates have huge uncertainty on them.
In theory, a lockdown will significantly reduce the spread of the disease outside the hospital setting, but without reliable estimates of the virus’s basic reproductive number, we don’t know whether such measures will be able to reduce the reproductive number below one. Similar measures taken in the SARS epidemic managed to cut the reproductive number to .4 within weeks of being instituted, so there is reason for optimism.
Similarly, hospitals, once mobilized, have had success at containing the inside-hospital spread of measles and ebola, so it is likely that with appropriate measures, the same will obtain in Wuhan and the epidemic will begin to shrink. But case numbers could rise very high before the epidemic’s growth is arrested, and there is a lot of uncertainty on this point.
How effective will the Wuhan quarantine be at limiting the spread of cases to regions outside Wuhan?
[Updated January 27, 9:42 pm]Not very effective! About 40% of the population of Wuhan bugged out before the quarantine, spreading well over a thousand cases all over China. There are already cases of Wuhan coronavirus in almost every province in China, and in many foreign countries. It’s likely more will be added rapidly in the coming days, as cases which spread before these current precautions are found.
Statistics from the Chinese government reveal that over five million people departed Wuhan for other parts of China in the last days before the quarantine and lockdown were instituted, and there have been sporadic, unreliable reports on Chinese social media of patients with fevers of unknown origin using antipyretic medicine to avoid the travel checks inside China in order to exit Hubei province.
Of course, the number of coronavirus patients arriving in locations outside Hubei and outside of China will be much reduced by such measures, but significant numbers of infected people have already left Hubei and China for a variety of destinations.
Most likely, the success of efforts to prevent widespread transmission of the coronavirus in areas outside Hubei province and outside China will depend on isolating and treating patients and preventing spread in those locations, rather than preventing any of them from arriving.
How effective will travel screening and quarantine of patients be at limiting the spread of cases into and within new countries?
We really don’t know. Such measures were effective at preventing significant transmission of SARS outside China, but ineffective at preventing a sizable MERS outbreak outside Saudi Arabia.
However, in both cases, the epidemic was rapidly contained even where the coronavirus began to spread. It is possible that significant transmission will not occur anywhere but Hubei province, but also possible that it will, and that other cities will shortly be facing their own widespread outbreaks. With the large number of unconfirmed cases in Hong Kong, it is possible that at least one city already is. Even if this happens, in one city or many, however, it is likely (based on historical precedent) that the epidemic can be arrested in each location.
What can we do about the next coronavirus, the next Ebola strain, or the next completely unknown virus?
This is a very difficult question, but there are a number of things we can do.
A year from now, or two, or five, when the Wuhan coronavirus outbreak has been eradicated, at whatever cost, humanity will once again be in a lull between outbreaks, this time having faced three deadly outbreaks in a twenty year period. Along, of course, with the emergence of HIV and the Ebola virus as brand new clades of human viral disease, unknown before they began killing. This fundamental situation is something that we will all be living with for the rest of our lives, and it suits us to take preparedness for this kind of thing more seriously than we do.
On the economic front, we can stop the market in wild animals sold for food with no safety precautions whatsoever. As a libertarian, I feel that people have a right to eat venomous snakes if they wish, but it should be a no brainer to sell venomous snake meat in appropriate sanitary conditions, and to test exotic meat from species with known disease vectors for disease before selling it. The situation wherein a hundred types of wild game are sold in the same dirty market with no precautions whatsoever is a tragic absurdity, and humans can do better, hopefully better enough to prevent the next coronavirus from breaking out this way.
On the biomedical front, there is a lot to do. Rapid genome sequencing and the ability to develop bespoke diagnostics very quickly, and share clinical information between clinics worldwide in a coordinated way, have done wonders in this and past coronavirus outbreaks. As biotechnology and communications improve, we can do better than that. We can also prototype methods for more rapid therapeutic design.
There is an NIH initiative afoot to design a tool compound for every protein in the human genome, in theory enabling drug target hypotheses to be tested much more rapidly. The same could be done for the genomes of known viral clades. And the technologies for drug and antibody design, as they continue to advance, should be kept ready to spring into action to develop new therapies against coronaviruses and other novel pathogens in an accelerated manner.
We can also develop therapies for known diseases. Antiviral therapies targeting the most conserved components of the coronavirus family should be developed and tested, including coronavirus vaccines, and plans to manufacture them at scale if needed should be established. The existing plans around Ebola preparedness should continue to move forward, so new outbreaks can be contained and exterminated faster. And of course, we should move beyond the current state of HIV research, find a cure for the disease, and eradicate the virus.
On the logistical front, we can expand our capacity to deploy field hospitals in areas affected by epidemic disease, convert hospitals from multipurpose to epidemic uses, and move healthcare workers and medicine and supplies into affected areas.
On the social front, we can expand our capacity to disseminate correct information about how people can protect themselves and check the spread of an ongoing epidemic, and build institutional honesty and the social trust that lets people have the confidence the information they receive is accurate and helpful, and lets people solve coordination problems like whether to leave crisis-stricken areas or shelter in place.
Some key infectious disease terms and concepts
Latency period: The period of time that elapses between the virus infecting one host organism, and the time at which that host organism will typically transmit its infection to others. Note that this is different from the incubation period: the time between an infection and the first symptoms.
Reproductive number: The average number of people who will become infected by transmission from one other person, over the life of an infection. The reproductive number of a virus in a largely uninfected population with little immunity, taking no special precautions, is referred to as a disease’s “basic reproductive number,” and may range from as low as 1.5 in an Ebola outbreak, to as high as 18 for a highly contagious virus like measles.
Case fatality rate (CFR): The percentage of infected hosts who die of the infection. This may range from a small fractional percentage for the common cold, through nearly 100% for untreated HIV infection. It varies considerably according to the quality of medical treatment received.
A brief history of recent coronavirus outbreaks
The SARS (Sudden Acute Respiratory Syndrome) coronavirus emerged in the Yunnan province of southern China in November 2002, spreading from horseshoe bats to humans, probably by way of civet cats eaten as food.
This theme, of viral reservoirs in animals making their way to humans by way of unusual forms of human-animal contact, is a recurring theme in viral outbreak news.
The SARS virus causes fever, respiratory symptoms, muscle pain, headaches, and other symptoms, and has a latency period of about 4-6 days, a basic reproductive number of about 2-4, and a case fatality rate around 10%. As you might expect from these parameters, the infection spread rapidly, resulting in several thousand cases by the time the WHO and local health authorities took effective control measures in April 2003. After this, the reproductive number dropped to about .4, and the outbreak was exterminated in June 2003.
Over the course of the SARS epidemic, 8,273 cases in 16 countries resulted in 775 deaths. Since then, despite a small number of individual isolated cases due to laboratory accidents, no additional SARS outbreaks have occurred.
The MERS (Middle Eastern Respiratory Syndrome) coronavirus emerged from bats by way of camels in Saudi Arabia in June of 2012. It causes symptoms similar to SARs, but with a higher proportion of serious cases, resulting in a higher case fatality rate above 30%. Its base reproductive number is lower than SARS, about 2.7, and largely confined to intimate contacts like household and medical connections, while its latency period is slightly longer in most cases.
The initial outbreak in Saudi Arabia grew slowly throughout 2013 and early 2014, followed by explosive growth in April 2014, which was largely controlled within a few months, and resulted in 1029 cases and 452 deaths. Despite the virus being largely controlled, residual cases spread to dozens of other countries, causing few problems in any of them, with the notable exception of an outbreak in South Korea which sickened 184 and killed 29 in May through July of 2015. This second outbreak is a potent reminder that when a particular outbreak has been controlled, it can rise again just as easily if the conditions which arrested it change, e.g. if it spreads to a new area or if control measures flag.
In the years since then, MERS outbreaks in camels have been seen in several countries, and a smaller MERS outbreak remains ongoing in Saudi Arabia since 2018.
These sudden and periodic coronavirus outbreaks have made coronaviruses a priority concern among epidemiologists, who warn that they constitute some of the greatest risks of a deadly large scale outbreak of any type of virus. This could come from the SARS or MERS coronaviruses, from a deadlier mutation of an endemic coronavirus, or from a novel coronavirus that catches us completely by surprise. In the case of the new Wuhan coronavirus, this latter scenario is exactly what happened.

You are reporting the comment """ by on